Today we’re going to finish Cardiac Drugs – here is our post from last week – http://www.nclexreviewonline.com/nclex-cardiac-drugs/
(Positive) inotropic agents: Increase force of myocardial contraction.
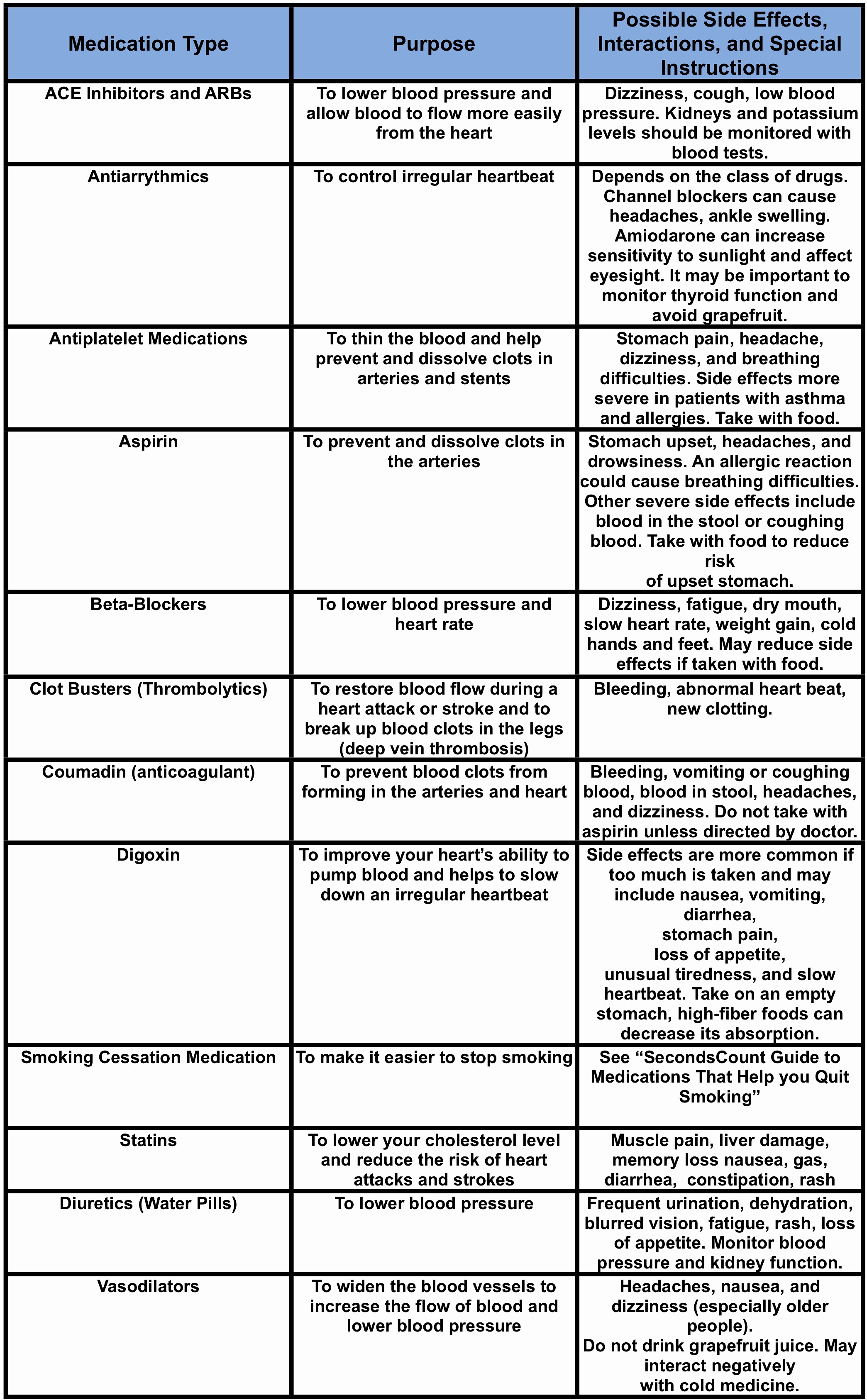
Digoxin (cardiac glycosides): Makes the heart beat slower, more regular and more powerful, which allows time for the ventricles to relax for better filling (increased diastolic filling).
Result: increased cardiac output and increased blood flow to the kidneys.
Adverse effects (digitalis toxicity): anorexia, N & V, visual disturbances, lethargy, bradycardia, heart block, tachydysrhythmias.
Take apical heart rate for one full minute before administering, noting rate and rhythm.
Monitor digoxin levels for toxicity: Dig has a narrow therapeutic window: 0.8-2.0 ng/ml.
Monitor potassium levels: Persons with hypokalemia are more likely to become dig-toxic so patient needs to eat foods high in potassium; Patients on Lasix and Dig – watch for toxicity.
Digoxin Immune Fab (Digibind) is antidote for Digitalis toxicity.
Sympathomimetic drugs: Stimulates beta1 receptors in the heart. Direct-acting cardiac stimulant.
Dobutamine: Stimulates beta1 receptors, increasing cardiac contractility, CO, and SV, with minor effects on HR.
Dopamine: Immediate precursor of epinephrine in the body. Produces direct stimulation of beta1 receptors and variable (dose-dependent) stimulation of alpha receptors (peripheral vasoconstriction). At low doses, increases blood flow to the kidneys.
Epinephrine: Causes marked stimulation of alpha, beta1, and beta2 receptors, causing cardiac stimulation, bronchodilation, and decongestion.
Digoxin Fab (Digibind)
Use: life-threatening digoxin toxicity
Mechanism: antibody complex formation to digoxin
Adverse events: Exacerbation of heart failure or a-fib due to withdrawal of digoxin; potential for complex dissociation with repeat toxicity in end-stage renal disease, hypersensitivity; digoxin levels meaningless for 7 days post Digibind use.
Morphine: For relief of chest discomfort unresponsive to nitroglycerin.
Relieves MI pain, decreases myocardial oxygen demand, reduces circulating catecholamines, reduces preload.
Adverse reactions: respiratory depression, hypotension, vomiting.
Potassium supplements: Maintains acid-base balance and electrophysiologic characteristics of the cell. Contraction of cardiac, skeletal, and smooth muscle.
Indications: Treatment of potassium depletion which may be caused by other medications or medical conditions.
Adverse reactions: Nausea, vomiting, stomach cramps (can be reduced by giving with food); tingling of hands, feet; confusion; unusual tiredness or weakness; heaviness or weakness of legs (contact doctor).
Nitrates (Vasodilators): Increases coronary blood flow by dilating coronary arteries and improving blood flow to ischemic regions of the heart. Also decreases preload by dilating peripheral veins.
Variety of routes: SL, IV, PO, TD
Used for angina, hypertension, MI, CHF.
Short-acting nitrates: Nitroglycerin: For acute anginal attacks. SL dosage (0.4mg):
– Instruct patient to lie down
– Repeat at 5 minute intervals; if pain not relieved, up to 3 tablets
– If anginal pain persists after 3 doses, call doctor or go to nearest ER
– Stay with patient and monitor VS (especially BP)
– Headache and hypotension are major side effects
Long-acting nitrates: Isordil, nitroglycerin ointment, nitroglycerin transdermal patch
– Non-hairy surface for patch
– Ointment: use appropriate application paper; don’t “rub in”
– Rotate sites (remove old patch, ointments)
– Avoid contact to your skin
– Nitrate-free periods (6 – 10 hrs/ 24 hr period) to prevent tolerance
– Remove patch before defibrillating as patch may explode
“MONA” greets everyone at the door. (with chest pain)
- Oxygen at 4 L/min
- Aspirin 160-325 mg (crushed or chewed)–antiplatelet action
- Nitroglycerin SL or spray–if BP > 90
- Morphine IV (2-4mg q5 min)–if pain not relieved with NTG
Pressor: something which causes the blood pressure to go up
Alpha pressor: pressorizes the arteries
Beta pressor: heart or lungs
ONE heart: Beta1
TWO lungs: Beta2
Alpha pressors tighten up the arteries by stimulating the alpha receptors in the arteries.
Beta pressors stimulate the beta1 receptors in the heart. This increases both heart rate and inotropy (contractility), which increases cardiac output and hopefully blood pressure.
+++++++++++++++
A great review (advanced) of heart drugs – it is from the UK but still valid – https://www.mheducation.co.uk/openup/chapters/9780335243976.pdf
+++++++++++++++
Next week we’ll have some study aids and questions.